Amakira
Preventing the risk of eating your own baby
The risk of eating your newborn baby
During my stay in Ndegeya, in central Uganda, I came across a special topic about mothers just after the birth of their baby. We know that it takes a lot of physical effort to deliver a healthy baby. But mental complications appear to be much more difficult to comprehend.
Mental illness is often viewed with fear and horror. For example, in Uganda, psychotic mental illnesses (eddalu) are attributed to bewitchment (Orley, 1970), or to vengeful ancestral spirits called Lubaale, with superhuman qualities that, if wronged, can haunt individuals of a clan by tormenting them with mental illnesses . (Nzita & Mbaga-Niwampa, 1997).
Many have heard of postpartum depression. This is a form of depression that can interrupt a mother's ability to bond with her baby. This affects about 1 in 8 mothers. A much worse condition is Postpartum Psychosis (PPP), also called puerperal psychosis, in which the mother's sense of reality changes after childbirth. Although the reasons are not fully understood, the symptoms are usually similar: paranoia, racist thoughts, delusions, an inability to sleep.
In this way she can harm herself or her children. In Central Uganda this was given the term Amakiro (Cox, 1979). In severe cases, people with Amakiro may try to kill themselves or their baby.
Sometimes the mother has a strong urge to eat her baby.
There are a number of factors that increase the risk of Amakiro:
- Medical factors, such as previous mental disorders and genetic predisposition;
- Psychosocial factors, such as lack of social support, difficult living conditions.
In Uganda, the psychosocial factors are so great that Amakiro is a well-known concept in the community.
However, Amakiro is treatable and early treatment increases the chance of a good outcome. A reason for the medical clinic in Ndegeya to take action.
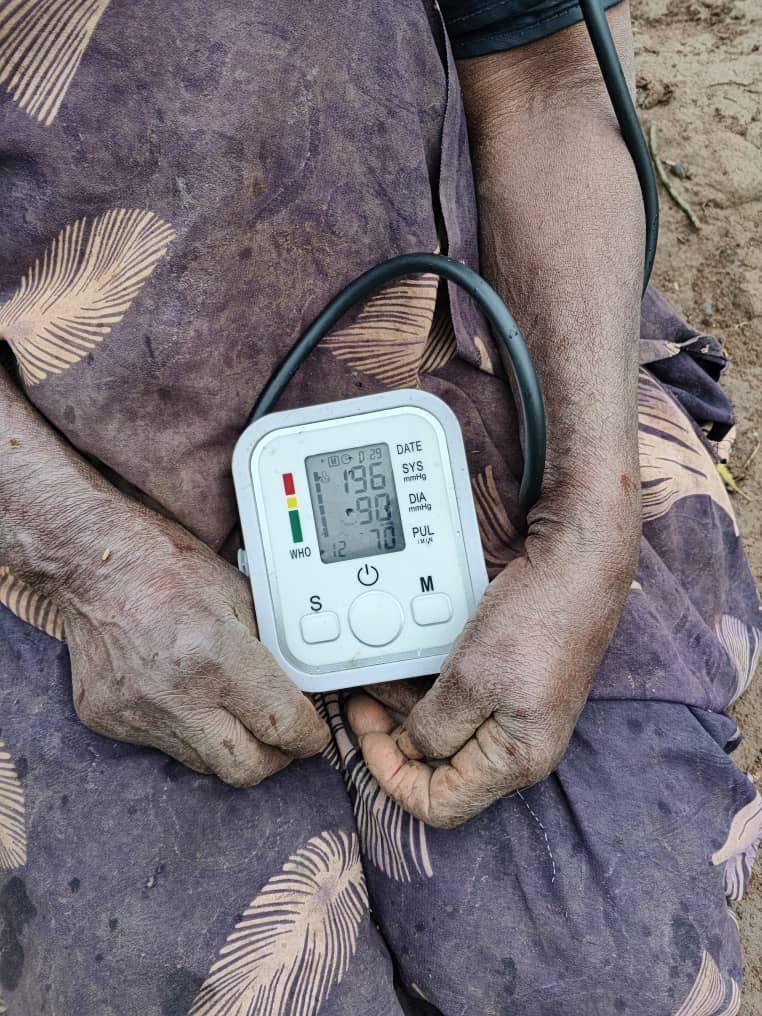
More than 6,000 people live in the Ndgeye community, the majority of whom have little or no food, medication or transportation and are dependent on the medical clinic set up by the Joanne Foundation. We are now working hard to set up a Mother and Childcare Center next to the clinic. The building is ready and the first pieces of furniture and equipment have been ordered.
What is needed now is to obtain the right medication for, among other things, mental health, such as antipsychosis and anti-epileptic medication, lithium, and mood stabilizers and equipment such as a mobile ultrasound scanner. In addition, a midwife must be hired and trained. This person can therefore help to develop and implement a workable program.
This center will focus on supporting pregnant women, helping with a safe delivery and ensuring that new mothers and babies get the help they need. By monitoring, providing timely information and, if necessary, giving the right medication, mothers and babies can be prevented from getting stuck at the start.
Share this post: